Written by Jack Ringer, DDS, FAACD, FIADFE
Introduction
Dentists can utilize a variety of technique options when it comes to fabricating provisional restorations for indirect therapy. The decision as to what technique and material to be used will be based on a variety of factors such as cost, durability, and esthetics.
This paper will address an efficient and inexpensive technique for fabricating extremely durable, yet highly esthetic, chair-side provisional restorations utilizing a unique bis-acrylic material called LuxaCrown (DMG). Most of today’s contemporary bis-acrylic provisional materials work well for single-unit restorations and even short-span bridges. However, for therapy requiring the patient to be in an esthetic provisional state for an extended duration (i.e. during implant therapy), these materials have a tendency to break, particularly for bridges. Historically, an option to overcome the issues with a long-term esthetic provisional was to have lab manufacture the provisional restoration utilizing lab-processed resins and in some cases, with metal reinforcement.
The obvious downside to this would be the elevated cost and time required to complete the process. Now, however, a new material allows the dentist to create a durable and esthetic chair-side provisional at a fraction of the cost.
Case Report
A patient returned to my office approximately four months after having six upper anterior teeth (#s 7-12) extracted and bone grafted (Figure 1). The patient had a previously unrestored implant for #13 along with existing old and defective full coverage crowns for #s 5, 6 and 14. (Figures 1 & 2). It was decided that teeth #s 5, 6 and 14 would have new ceramic crowns, and following implant placement, an all-ceramic bridge would be placed in #5 – 12 location as well as a separate crown for #13. Because it would take several more months to complete the treatment process, creating an esthetic and durable provisional for this period of time would be critical.
Once the patient had the teeth extracted and the sites bone grafted, she returned to my office to have her custom provisionals fabricated. As with any case that involves an esthetic makeover, a smile design (i.e. a computer simulation and custom wax up) was created first. A putty stint was fabricated by my assistant off of the proposed diagnostic wax up (Figure 2).
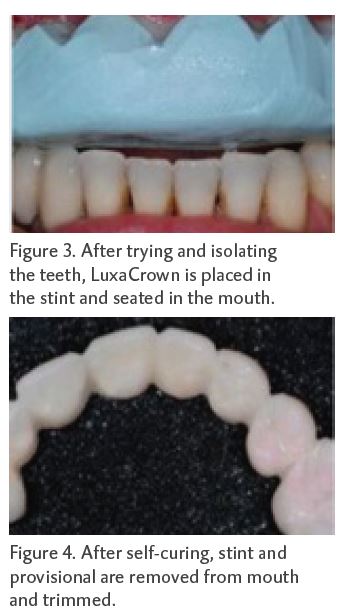
The stint was tried in to ensure it seated well and teeth #s 5, 6 and 14 were preliminarily prepared for new full coverage restorations. The teeth were then dried and isolated and LuxaCrown (a B1 shade for this patient) was placed in the stint and seated in the mouth (Figure 3). After it self-cured, the stint and the provisional were removed from the mouth and the provisional was trimmed (Figure 4). The provisional was then tried back in the mouth, and minor fine trimming, adjusting and bite adjustments were performed. Once the size, shape and fit were confirmed, the provisional was polished and luted in the mouth. Because the provisional’s fit was very snug, a provisional cement was used. The fit, contour and esthetics of the final provisional met both the patient’s and the dentist’s expectations (Figure 5).
Discussion
The use of a provisional cement allows a surgeon to safely and easily remove the provisional to access the extraction sites, or at a later date, place the implants. The provisional can then be easily re-cemented. One other advantage to this technique is that it allows the dentist to make modifications (i.e. adding resin) during the course of the therapy. In this case, it will be necessary as the tissue remodels during the healing phase, which will leave large spaces gingivally if not corrected. Be it for porcelain laminates, crowns, bridges or implant therapy, the provisional protocol is the same as that described in the clinical case above.
In this case, the dentist and patient can have great confidence that this long span LuxaCrown bridge will maintain its integrity and appearance during the course therapy, provided the patient is diligent with hygiene and does not abuse the provisional by exerting it to unnecessary occlusal or traumatic forces.