Written by Dr. Hugh Flax, DDS, AACD, MICOI, DABAD
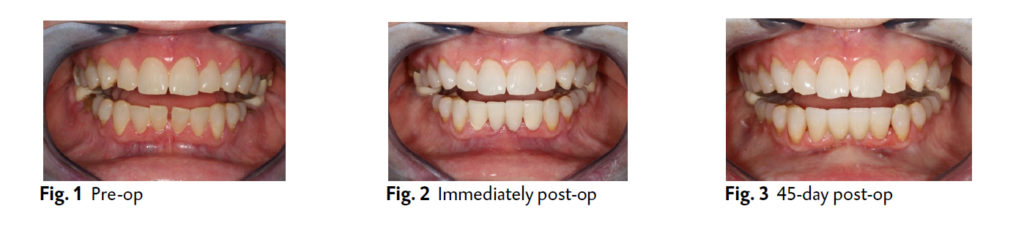
A 65-year-old woman was finding it increasingly difficult to bite on her front teeth. Additionally, she had noticed increasing spacing between her lower incisors (Fig. 1). Her exam revealed severe bone loss around teeth #24 and #25 with class 3 mobility and secondary occlusal traumatism. The prognosis was that it was impossible to save the teeth, and atraumatic removal was recommended. Treatment planning with a CBCT showed a damaged buccal plate that would compromise immediate implant placement and require 2 stage grafting/implant surgery. The patient wanted a stable fixed transition solution while healing. It was determined that an ovate pontic design would preserve the gingival architecture by providing a “scaffold” to prevent collapse and flattening of the papillae.
A well designed and sculpted putty matrix was provided by the laboratory. The patient was given a sedative dose of Xanax. Eight vials of blood were drawn to create a mix of PRGF and 50/50 mix of cortical/decortical bone. Teeth #23 and #26 were prepared for a fixed transitional bridge. The central incisors were atraumatically luxated to spare any remaining bone, and the sockets were carefully debrided and irrigated with sterile saline.
LuxaCrown semi-permanent crown and bridge material was injected into the putty matrix and intraorally around the gingival tissues to create precise margins and ovate pontics. The prosthesis was shaped with discs and composite finishing burs. It was readily apparent that the material’s firmness reflected its higher density. Occlusion was refined in centric and eccentric positions. Final polishing was done with 3 grits of discs and aluminum oxide paste and the bridge was placed in Peridex. Following socket bone stimulation, the intraosseous bone graft was placed and packed into the extractions sites. Figure eight suturing with self-resorbing 4-0 polyglycolic acid was performed to hold the tissues and graft material stably for 60-90 days. The restoration was cemented after coating the preparation with a disinfectant and desensitizer, followed by a reversible cement.
The patient was ecstatic about the esthetic and functional improvement of her lower teeth (Fig. 2). The stability and firmness gave her and her dental team the peace of mind that the prosthesis would be durable during the healing and implant care processes. The high polish and precise adaptation around the tissues enabled the papillae to remain intact at the 45-day mark (Fig. 3). Such an outcome was not possible with standard provisional crown and bridge materials.
GO-TO PRODUCT USED IN THIS CASE
LuxaCrown Long-Term Crown and Bridge Material
DMG’s LuxaCrown is the chairside way to long-lasting crowns, thereby providing valuable time and cost savings for patients and clinicians. It can deliver a long-term restoration that is long-lasting, with excellent fracture toughness and flexural strength. LuxaCrown can be used with a quick, easy technique and exhibits optimal mechanical properties and exceptional polishability and versatility of applications.
Hugh D. Flax, DDS, AACD, MICOI, DABAD A 1983 graduate of Emory University School of Dentistry, Dr. Flax has been a member of the American Academy of Cosmetic Dentistry since 1994 and became accredited in 1997. He is a past President of the Atlanta Chapter of the AACD and founded the Georgia Academy of Cosmetic Dentistry in 2007. He is on the Editorial Board of the Journal of Cosmetic Dentistry and Practical Periodontics and Restorative Dentistry. Dr. Flax is also a certified Fellow with World Clinical Laser Institute and a clinical Instructor at Georgia Regents University College of Dental Medicine. A frequent clinical writer and lecturer, Dr. Flax practices full time in Atlanta, Georgia focusing on functional-appearance related conditions and advanced laser dentistry.
